
Our Office
Visit Us Online
-
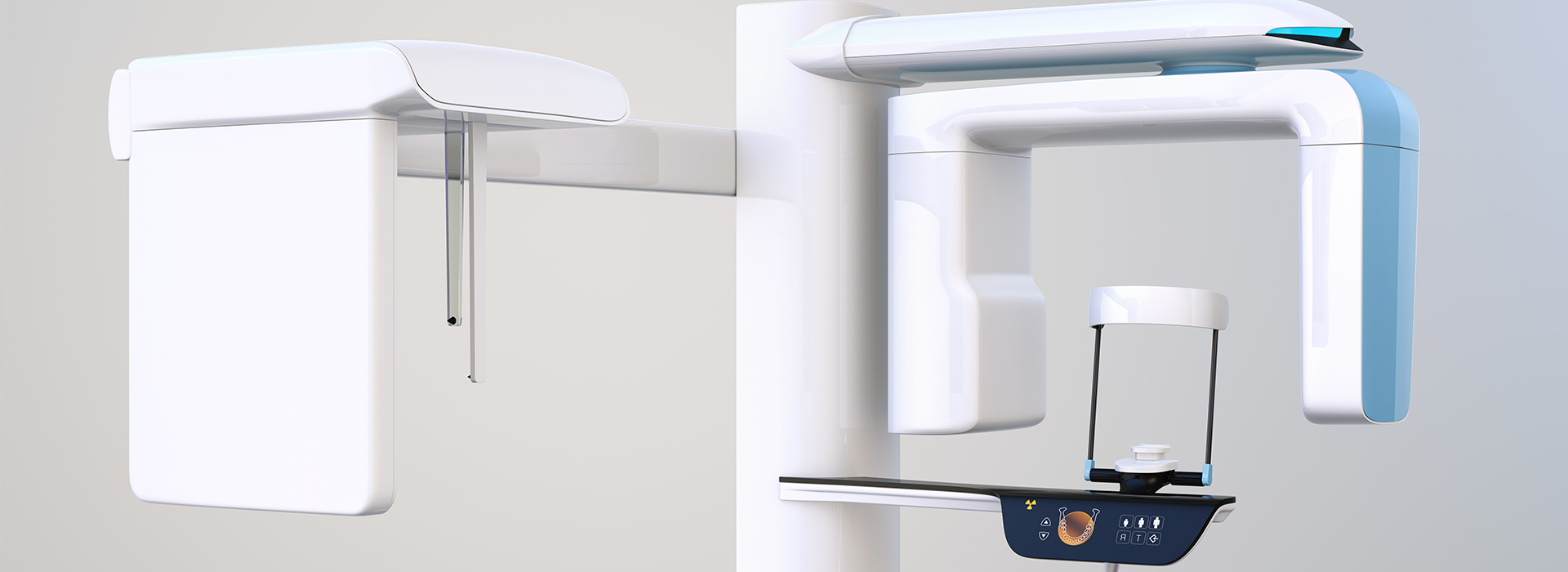
At the office of Morrison Dental Care, we embrace advanced imaging to help clinicians see more clearly and plan more precisely. Cone-beam computed tomography (CBCT) converts X-ray data into detailed three-dimensional views of teeth, jaws, and surrounding structures, giving dentists the kind of spatial information that conventional two-dimensional films cannot provide.
CBCT is a diagnostic tool, not a treatment in itself. When used thoughtfully, it supports better decision-making across restorative, surgical, and diagnostic care — improving predictability while preserving patient comfort and safety. The sections below explain what CBCT reveals, how it supports treatment planning, and how we integrate it into everyday practice.
Traditional radiographs compress complex anatomy into a flat image. CBCT overcomes that limitation by producing volumetric datasets that present teeth, bone, nerves, sinus cavities, and soft-tissue outlines in three dimensions. This perspective helps clinicians evaluate depth, relationships, and angulation with far greater clarity.
For example, bone volume and density can be assessed throughout the jaw rather than inferred from a two-dimensional slice. Nerve pathways and the position of the maxillary sinuses become apparent in multiple planes, reducing guesswork and enabling more precise risk assessment before invasive procedures.
CBCT also picks up subtle anatomic variations and pathology that can be missed on standard films. Small cysts, complex root anatomy, and localized bone defects are more readily identified, which allows the clinician to tailor the treatment approach and anticipate potential complications.
Dental implant success depends on accurate planning and precise placement. CBCT provides a roadmap for implant therapy by revealing the three-dimensional relationship between proposed implant sites and critical structures such as the inferior alveolar nerve, the mental foramen, and the floor of the sinus.
With CBCT data, clinicians can evaluate bone height, width, and quality at the intended implant site, determine optimal implant length and diameter, and identify areas that might require grafting. The information supports selection of the proper implant position to achieve stable, long-term results while avoiding vital anatomy.
Many modern implant protocols take advantage of CBCT-derived surgical guides and virtual planning. By combining the CBCT dataset with restorative planning, we can create predictable, prosthetically driven implant placements that streamline surgery and improve the fit and function of the final restoration.
Beyond implantology, CBCT has become a valuable tool in endodontics for diagnosing complex root canal systems, locating accessory canals, and identifying periapical pathology. When a tooth’s anatomy is unclear on conventional films, a targeted CBCT scan can reveal root curvature, fractures, and resorptive defects that alter treatment strategy.
In airway and sleep-related assessments, CBCT enables visualization of the upper airway space in multiple planes. Measuring airway volume and identifying areas of constriction helps clinicians collaborate with medical colleagues and design interventions that address structural contributors to sleep-disordered breathing.
Temporomandibular joint (TMJ) concerns also benefit from three-dimensional imaging. CBCT provides clear views of condylar morphology, osseous changes, and joint space relationships, aiding in the detection of degenerative changes or developmental abnormalities that may influence treatment planning.
Radiation exposure is an important consideration for any X-ray–based technology. Contemporary dental CBCT units employ pulsed exposures, collimation, and selective fields of view to limit radiation to the area of clinical interest. When used according to the ALARA principle — “as low as reasonably achievable” — CBCT delivers diagnostic benefit while minimizing dose.
Clinicians choose the smallest effective field of view and the appropriate resolution for each clinical question. For many focused applications — such as a single-root assessment or localized implant site review — a limited-volume scan provides excellent diagnostic value with substantially lower exposure than a full-arch study.
Patient comfort is also a priority. Scans are brief, typically completed in a matter of seconds to a minute depending on the device and protocol, and most patients find the experience straightforward and noninvasive. Clear communication before the scan helps patients relax and remain still, which improves image quality.
Producing clinically useful CBCT information requires more than obtaining a scan; it involves consistent protocols for acquisition, image review, and interpretation. Our workflow begins with a focused clinical question: what do we need to know to guide treatment? That question determines the scan parameters, the field of view, and the reconstruction settings.
Once the dataset is acquired, digital tools allow multiplanar reconstructions, cross-sections, and three-dimensional renderings that can be rotated and measured. These features support objective analysis — for example, measuring bone thickness, evaluating angulation, or determining the proximity of implants to neural structures — which enhances communication between the dentist, specialists, and laboratory partners.
CBCT datasets can be exported to design software for surgical guide fabrication, to CAD/CAM systems for restorative planning, or to referral specialists for collaborative care. This interoperability accelerates treatment timelines and helps ensure everyone involved in a patient’s care works from the same detailed diagnostic information.
In summary, cone-beam computed tomography is a powerful diagnostic resource that elevates clinical understanding, supports more predictable outcomes, and integrates seamlessly with modern digital dentistry. When selected and interpreted appropriately, CBCT contributes meaningfully to safer, more effective treatment planning across restorative, surgical, and diagnostic applications.
If you’d like to learn more about how CBCT may benefit your care or to discuss whether advanced imaging is appropriate for a particular treatment, please contact our office for more information.
Cone-beam computed tomography (CBCT) is a three-dimensional imaging technique that captures detailed volumetric views of the teeth, jaws and surrounding facial structures. It uses a cone-shaped X-ray beam and a digital detector to reconstruct cross-sectional images in multiple planes, producing a single 3D data set. This advanced modality provides precise anatomic detail that supports diagnosis and treatment planning for complex dental cases.
Unlike traditional two-dimensional dental X-rays, CBCT delivers volumetric information that shows depth and spatial relationships between structures. Clinicians can visualize bone contours, nerve pathways and sinus anatomy with greater accuracy, which reduces ambiguity in interpretation. As a result, CBCT often enables more informed and predictable treatment decisions.
CBCT is used across many specialties, including implant planning, assessment of impacted or supernumerary teeth, endodontic evaluation of complex root canal anatomy and detection of bony pathology. It is also valuable in orthodontics for evaluating tooth position and jaw relationships, and in oral surgery for preoperative planning. The high-resolution 3D data support multidisciplinary workflows where exact anatomy matters.
When combined with digital impressions and planning software, CBCT data can be used to design surgical guides, determine optimal implant angulation and assess the need for bone grafting. It also assists in diagnosing cysts, tumors and other maxillofacial abnormalities that may be difficult to appreciate on standard films. Clinicians rely on this information to tailor treatment to each patient’s unique anatomy.
CBCT uses ionizing radiation, but modern dental CBCT machines and optimized protocols are designed to limit exposure while delivering diagnostic-quality images. Effective dose varies with field of view, resolution settings and scan time, so clinicians select the smallest volume necessary for the diagnostic task. Compared with medical CT, dental CBCT typically involves a substantially lower radiation dose for comparable anatomic regions.
Dentists adhere to the ALARA principle (as low as reasonably achievable) when ordering imaging, and CBCT is recommended only when the expected diagnostic benefit will influence care. Protective steps such as reducing field of view, adjusting exposure parameters and ensuring proper patient positioning further reduce dose. Your clinician can explain why CBCT is advised in your case and how the expected benefits outweigh the minimal risks.
CBCT provides three-dimensional measurements of bone height, width and density, enabling precise evaluation of potential implant sites and identification of anatomic limitations. Visualization of the mandibular canal, mental foramen and maxillary sinus helps avoid nerve injuries and sinus complications during implant placement. This detailed assessment supports confident selection of implant size, position and the need for augmentation procedures.
When CBCT data are integrated with digital impressions and surgical guide software, the virtual plan can be translated accurately to the surgical field. This coordinated workflow improves predictability, often reduces operative time and enhances prosthetic outcomes. Patients benefit from more accurate restorations and a decreased likelihood of unexpected intraoperative findings.
A CBCT scan is generally quick and noninvasive, with the actual image acquisition often completed in less than a minute. The patient sits or stands while the scanner rotates around the head, and simple positioning aids help maintain comfort and alignment. There is no need for intravenous contrast or sedation for routine dental CBCT exams.
Preparation is minimal; patients may be asked to remove glasses, jewelry and removable dental appliances that could cause artifacts. After the scan the images are reconstructed into a 3D volume that the dentist reviews, frequently during the same visit or shortly thereafter. Your clinician at Morrison Dental Care will discuss the findings and the recommended next steps based on the CBCT results.
Preparation for a CBCT scan usually involves removing metal objects such as earrings, necklaces and removable prostheses that can create imaging artifacts. Pregnant patients should inform the dental team, since imaging during pregnancy is generally avoided unless absolutely necessary and justified by a clinician. Children and patients who have difficulty remaining still may require additional positioning support or shortened scan protocols to optimize image quality.
Patients with limited mobility or certain medical conditions should discuss these issues with the dental team so appropriate accommodations can be made. If CBCT is not feasible or the anticipated information would not alter treatment, alternative imaging options may be considered. Clinicians perform a case-by-case risk-benefit assessment to select the most appropriate imaging modality for each patient.
Dentists and oral surgeons analyze CBCT volumes using specialized software that allows multiplanar reformatting, cross-sectional slicing and three-dimensional rendering. These tools enable precise measurements, evaluation of bone morphology and visualization of relationships between teeth, nerves and sinuses. For complex findings, many practices consult with oral and maxillofacial radiologists or specialists to ensure a comprehensive interpretation.
The diagnostic information from CBCT informs surgical guides, implant placement strategies, endodontic approaches and orthodontic treatment sequencing. Clear visualization of anatomic detail reduces intraoperative surprises and supports evidence-based decision making. Final treatment plans integrate CBCT findings with the clinical exam, patient goals and other diagnostic tests for a holistic approach to care.
Yes. Because CBCT produces volumetric images, it can reveal pathologies and anatomic details that may be obscured or superimposed on two-dimensional radiographs. Small fractures, accessory canals, root resorptions and localized bone defects can be more readily identified on CBCT than on panoramic or periapical films. This additional information may alter the diagnostic impression and influence treatment choices.
CBCT is particularly useful for assessing the extent of bony lesions, the precise position of impacted teeth relative to adjacent structures and subtle sinus abnormalities. However, not every clinical question requires CBCT, and clinicians determine its necessity based on whether the results will change patient management. When used appropriately, CBCT enhances diagnostic accuracy and clinical confidence.
CBCT provides detailed views of the bony components of the temporomandibular joint, allowing assessment of condylar morphology, joint space and degenerative changes. For airway evaluation, CBCT can visualize upper airway volume and areas of constriction that are relevant to sleep-disordered breathing. These objective anatomic data complement clinical examination and functional assessments.
Because CBCT primarily images hard tissues, complementary tests such as MRI for soft-tissue evaluation or polysomnography for sleep studies may be needed for a complete assessment. Dentists integrate CBCT findings with patient history, clinical signs and specialist input to develop multidisciplinary care plans. This combined approach improves diagnostic precision for TMJ disorders and airway management.
Morrison Dental Care follows established imaging protocols, regular equipment maintenance and staff training to ensure consistent image quality and patient safety. The practice applies ALARA principles by selecting the appropriate field of view and exposure settings for each diagnostic need and documents the clinical justification for CBCT use. Routine quality assurance checks and timely software updates help maintain diagnostic reliability.
Patients receive clear explanations about why CBCT is recommended, what to expect during the scan and how the images will be incorporated into their individualized treatment plan. When a case would benefit from additional expertise, the practice consults with specialists or oral and maxillofacial radiologists to confirm findings and refine treatment recommendations. These steps ensure that CBCT contributes meaningfully to safe, effective dental care.
Address:
1524 Route 9, Clifton Park, NY 12065